On March 2nd, 2010 I returned to work with my twice former employer HealthInsight, the highly regarded long-standing not-for-profit Medicare QIO (Quality Improvement Organization) serving the states of Utah and Nevada in the wake of their being awarded a federal "Regional Extension Centers" (REC) contract by the U.S. Department of Health and Human Services (HHS) as part of the Obama administration's stimulus funding initiative to spur the widespread adoption and "meaningful use" (MU) of health information technology (HIT).
On March 2nd, 2010 I returned to work with my twice former employer HealthInsight, the highly regarded long-standing not-for-profit Medicare QIO (Quality Improvement Organization) serving the states of Utah and Nevada in the wake of their being awarded a federal "Regional Extension Centers" (REC) contract by the U.S. Department of Health and Human Services (HHS) as part of the Obama administration's stimulus funding initiative to spur the widespread adoption and "meaningful use" (MU) of health information technology (HIT).
It is a most ambitious, pedal-to-the-metal, high-velocity program (unrealistically so, say some of its critics), one whose goal is to bring the vast majority of medical providers into the digital information world, a world the rest of commerce finds at once unremarkable and indispensable.
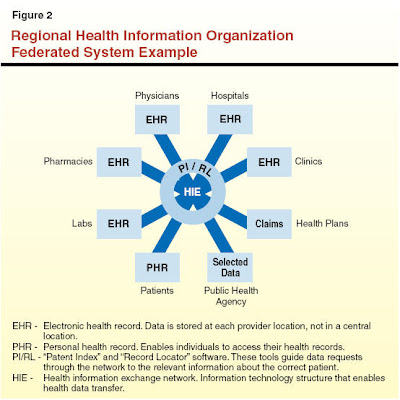
 Above, the still-predominant information storage and retrieval model for medical information. It is functionally untenable. Prohibitively expensive in ways significantly under-appreciated. It is dangerous. It could cost you your life in an exigent circumstance. It cries out for extinction. Yes, conversion will be difficult, and exasperatingly rife with logistical and legitimate, vexing policy problems.
Above, the still-predominant information storage and retrieval model for medical information. It is functionally untenable. Prohibitively expensive in ways significantly under-appreciated. It is dangerous. It could cost you your life in an exigent circumstance. It cries out for extinction. Yes, conversion will be difficult, and exasperatingly rife with logistical and legitimate, vexing policy problems.
Nonetheless...
 I have been writing a bit about this on one of my other blogs. See "Irrespective of national health care policy reform legislation, the medical sector is going full-steam-ahead HITECH," initially written prior to the passage of the Obama "Health Care Reform" legislation (with updates still to ensue, mostly pertaining to the complex data security issues bearing on patient privacy).
I have been writing a bit about this on one of my other blogs. See "Irrespective of national health care policy reform legislation, the medical sector is going full-steam-ahead HITECH," initially written prior to the passage of the Obama "Health Care Reform" legislation (with updates still to ensue, mostly pertaining to the complex data security issues bearing on patient privacy).
ASQ
The American Society for Quality. My wife and I have been members since the mid-1980's. We live and breathe "quality" concepts and issues, having both come together out of the same legacy-era "quality control" paradigm. We have both served as Examiners for our Nevada state-level Baldrige Award assessments (ASQ administers the national Baldrige program). My friend and ASQ colleague Fred Schwager and I co-founded the Nevada Quality Alliance (NvQA.org), which administers the Nevada Baldrige model program.
 When I returned to work, I renewed my optional special interest sub-membership in the ASQ Health Care Division. Shortly thereafter, I had the fine fortune to strike up an internet and phone conversation with the Chair-Elect of the Division, Dr. Joseph Fortuna. Joe is an enthusiastic supporter of the REC effort, and was intimately involved in DC legislative support for health policy reform.
When I returned to work, I renewed my optional special interest sub-membership in the ASQ Health Care Division. Shortly thereafter, I had the fine fortune to strike up an internet and phone conversation with the Chair-Elect of the Division, Dr. Joseph Fortuna. Joe is an enthusiastic supporter of the REC effort, and was intimately involved in DC legislative support for health policy reform.
We share some concerns, which we have by now discussed at some length; e.g.,- Critics bemoan a lack of prior HIT deployment and QI experience among some REC awardees (as well as the heterogeneity of business models);
- While 60 REC contracts have thus far been awarded, with the newly chartered RECs frantically ramping up to meet the rather compressed Stage One Meaningful Use incentive payment timelines, both the requisite Meaningful Use reporting criteria and the EHR (Electronic Health Record) certification regulations remain unresolved at this writing. The cart is seriously out in front of the horses in many respects;
- Notwithstanding that HHS is spending hundreds of millions of dollars on REC contracts, physicians and hospitals are not required to engage REC services in order to qualify for federal incentive payments. Consequently, RECs are having to spend significant time and money hawking their services (the polite term being "enrollment." I did not know when I signed on that I would be required to do what amounts to hastily and minimally trained cold-call sales). Moreover, REC services are not fully subsidized, the upshot of which is often skeptical "we'll pass" pushback, especially in light of the hyperbolic claims of virtually all major EHR vendors "guaranteeing" that their products will get the provider to MU (with the glossed-over disclaimer, well down in the fine print "When Used As Directed");
- At this writing, the aggregate Final Rule for MU criteria is still under HHS consideration, with myriad professional stakeholder groups arguing for relaxation of both the compressed compliance timelines and the all-or-nothing approach, countered by a broad array of equally vocal consumer/patient advocacy organizations arguing for MU criteria adoption "as-is" as set forth in the Interim Final Rule.
I would have added another MU criterion: require working with the RECs as a condition of incentive money eligibility;
- The relatively sparse per-provider federal REC funding may force the RECs to focus simply on assisting their client physicians with hitting the MU criteria in pursuit of the incentive reimbursements -- to the practical exclusion of broader and more sustainable, internalized quality improvement efforts;
- There is to be a "Health IT Research Center" funded by HHS and intended to "gather relevant information on effective practices from a wide variety of sources across the country and help the Regional Extension Centers (RECs) collaborate with one another and with relevant stakeholders to identify and share best practices in EHR adoption, effective use, and provider support. The HITRC will build a virtual community of shared learning to advance best practices that support providers’ adoption and meaningful use of EHRs."
It is not even slated to be up and running until FY2012.
Notwithstanding our concerns, we see potential opportunities for win-win synergistic REC-ASQ collaboration via which to help improve health care.
THE ASQ HEALTH CARE DIVISION "MARSHALL PLAN"
 Dr. Fortuna is a Champion of the ASQ "Marshall Plan."
Dr. Fortuna is a Champion of the ASQ "Marshall Plan.""...In different areas of the country, ASQ members, under the leadership of the ASQ Healthcare have teamed up with the local healthcare community and medical organizations to help improve healthcare delivery. Being that we are all stakeholders in this system and that there is much opportunity to apply quality and lean methodologies, this is a great place for ASQ members to use their skills for the betterment of the system. The focus is on primary care doctor offices..."
___
Click the link, Read all of it. An extremely worthy volunteer effort with the potential to deploy a large number of experienced QI professionals in pro bono service to the healthcare community in a manner complementary to and reinforcing of the work of the RECs.
The Regional Extension Centers could certainly benefit from the help, and ASQ in return would be made visible to a large source of potential new members, given the projected HIT-related and health professions employment growth across the decade.
I would also favor inviting several other ASQ Divisions to collaborate: Biomedical, Software, and Service Quality.



There is a lot of experience and relevant expertise upon which to draw. I would even surmise there might be interest and value adding input from and collaboration with the ASQ Quality Management and Statistics Divisions.
___
"LEAN? THAT MAY BE OUT OF OUR SCOPE"
Such was a reaction from one of my skeptical HealthInsight HIT Adoption Support team members during a recent meeting in which I'd recommended that we consider deploying aspects of "lean methods" for workflow analysis and re-design, as proffered most recently in the new Quality Press book "Lean Doctors." He didn't say so explicitly, but his implication was clear: in light of our finite FTE resources and the huge scope of the project, our necessarily circumscribed task will be to drive providers toward MU and the incentive money riding on it [PDF], period. Point taken, to an extent, but, it should be equally clear that I don't regard the MU goal contractual imperative as inexorably being at odds with the utility of lean re-design tactics. Neither do I buy the implicit, gauzy HHS assumption that clinicians hitting the MU targets amid the money chase constitutes focused, adequate, and lasting healthcare QI of the kind we are incontrovertibly in need of.
 This (highly recommended) book rightly points out, ever so politely, that the term "workflow" -- particularly in the medical setting, can be seen as having become something of a cliche, i.e., there's typically very little in the way of smooth "flow" in the daily "work," which is more aptly typically characterized as a series of "push" processes rife with bottlenecks caused by lack of coordination and waste. Any method that can demonstrably abate that simply has to be worthy -- whatever you choose to call it.
This (highly recommended) book rightly points out, ever so politely, that the term "workflow" -- particularly in the medical setting, can be seen as having become something of a cliche, i.e., there's typically very little in the way of smooth "flow" in the daily "work," which is more aptly typically characterized as a series of "push" processes rife with bottlenecks caused by lack of coordination and waste. Any method that can demonstrably abate that simply has to be worthy -- whatever you choose to call it.
In the words of the publisher's blurb, Lean Doctors posits
"six proven “success steps” for implementing lean in any healthcare environment:
- Create physician flow
- Support physician value-added time
- Visually communicate patient status
- Standardize everyone’s work
- Lay out the clinic for minimal motion
- Change the care delivery model
"Why go through such a transformation? Because it works. Tell a doctor that he can see the same number of patients, offering the same high quality and personal care, and have an extra 90 minutes at the end of his clinic day – and that means something. Tell the staff that they can look forward to actually ending on time, with satisfied patients, no backlog, and having focused their attention completely on quality patient care – and they will listen..."
"They will listen." Really? Making that sale is perhaps not as easy as it might appear. But, in my view, such is our mandate, given that the elimination of process flow roadblocks and the waste they comprise cannot but provide, among other QI benefits, the availability of the requisite time for MU compliance.
A useful quote from the text for now:
Lean is a science for creating flow in a system—whether of a physical product or of a service. In healthcare, this would mean that we aim to create patient flow, without wait times, through any given area. As we focused on patient wait times in the clinic we found that no other metric brought the varied root causes of inefficiency so clearly into focus. When patients were moving through the process promptly, a lot of things were going right. However, when patients waited in the exam rooms or waiting rooms or at supplying processes, then any one of a great number of things could be going wrong...
And, one more:
As you consider undergoing a Lean transformation process at your own practice or clinic (or hospital or larger healthcare setting), you might think that a minute shaved off here and a minute saved there does not seem worth much. Change is difficult, time-consuming, and cumbersome. So why would you literally analyze every step a nurse takes? Why take the time to have technicians or nurse practitioners describe in detail the reality of their jobs, when you need them to simply get the work done? Why? [again] Because it works...
Color me a believer, based on what I have thus far learned. However, our REC reality may be that we will largely be limited to predominantly a prescriptive/advisory/auditing role. We will necessarily be developing SOPs via which to guide clinicians and their staffs toward accurately and routinely documenting in their EMR systems the structured data required for their MU Stage 1 attestations (and eventual data reporting). The current draft of MU criteria contains 25 outpatient items, many of which require numerator and denominator data for calculating percentages that must meet or exceed MU thresholds, e.g.,
- 1.01 Computerized Physician Order Entry (CPOE): Use computerized CPOE for at least 80% all orders (e.g. medications, consultations, labs, diagnostic imaging, etc.);
- 1.02 Medication Interaction/Contraindication Checks: Enable functionality in EHR for automated drug-drug, drug-allergy, and drug-formulary checks;
- 1.03 Patient Problem List: Maintain an up-to-date problem list of current and active diagnoses (recorded as structured data) based on ICD-9-CM or SNOWMED CT® for at least 80% of all unique patients;
- 1.04 E-Prescribing: At least 75% of all permissible prescriptions written are transmitted electronically (eRx) using an EHR;
- 1.05 Active Medication List: Maintain an active medication list (recorded as structured data) for at least 80% of all unique patients;
- 1.06 Active Medication Allergy List: Maintain an active medication allergy list (recorded as structured data) for at least 80% of all unique patients;
- 1.07 Patient Demographics: Record demographic data (including preferred language, insurance type, gender, race and ethnicity coded by federal guidelines, and date of birth) as structured data for at least 80% of all unique patients;
- 1.08 Vital Signs: Record and chart vital signs (including height, weight, blood pressure, calculated and displayed BMI, plotted and displayed growth charts for children) for at least 80% of all unique patients;
- 1.09 Smoking Status: Record smoking status for at least 80% of all unique patients 13 years old or older;
- 1.10 Lab Results: Clinical lab results captured as structured data for at least 50% of all labs ordered...
...and so forth. SOPs driving toward uniformly capturing such subsequently queryable information will necessarily be EMR platform-specific, and will comprise substantial work to derive and implement. Consequently, I may in fact be asking too much to insist on inclusion of "Lean" principles in our REC workflow re-design effort during this initial phase.
But, before I leave this issue (regarding which I welcome commentary/feedback), consider a few screen clip excerpts from a recent Lean project study posted on the ASQ Healthcare Division web page:



 While I know that a lot of QI has gotten a sometimes deserved rep of being "soft" touchy-feely dubious flip-chart fad-of-the-moment social "science," the outcomes here are expressed in (verifiable, I assume) bottom line "hard dollar annual savings" on the order of $90k.
While I know that a lot of QI has gotten a sometimes deserved rep of being "soft" touchy-feely dubious flip-chart fad-of-the-moment social "science," the outcomes here are expressed in (verifiable, I assume) bottom line "hard dollar annual savings" on the order of $90k.
Annual.
Now, consider: the maximum HHS MU physician incentive payments are $44,000 over 5 years for Medicare providers and $63,750 over 6 years for Medicaid providers.

 Think about that, in the context of leaning up one process at a net of 90 grand a year.
Think about that, in the context of leaning up one process at a net of 90 grand a year.
The basic issue, visually:
 More to come...
More to come...
___
 I am aghast, angry, and depressed over the events in the Gulf of Mexico that began with the catastrophic, tragic fiery destruction of the British Petroleum Deep Water Horizon oil drilling platform and the unimaginably horrific deaths of eleven of its workers.
I am aghast, angry, and depressed over the events in the Gulf of Mexico that began with the catastrophic, tragic fiery destruction of the British Petroleum Deep Water Horizon oil drilling platform and the unimaginably horrific deaths of eleven of its workers. This will very likely turn out to be far and away the most severe man-made environmental calamity of my lifetime. The Gulf of Mexico (and perhaps far beyond) faces biological and economic ruination that may well be at this point beyond human capacity to truly remediate.
This will very likely turn out to be far and away the most severe man-made environmental calamity of my lifetime. The Gulf of Mexico (and perhaps far beyond) faces biological and economic ruination that may well be at this point beyond human capacity to truly remediate.
 Six chambers, one live round. Place your bet, load the weapon, spin, place the business end of the barrel against your temple, pull the trigger. The probability of blowing your brains out in the wake of each attempt is one in six. Would you do it?
Six chambers, one live round. Place your bet, load the weapon, spin, place the business end of the barrel against your temple, pull the trigger. The probability of blowing your brains out in the wake of each attempt is one in six. Would you do it? No need to idle all those drillers. There's plenty of heavy industrial work to be done.
No need to idle all those drillers. There's plenty of heavy industrial work to be done.